 By Peter Louis Glickman, M.D.
By Peter Louis Glickman, M.D.
All-American Teleradiology
Finger pulleys are fine annular and cruciform structures, which hold the flexor tendons close to the phalanges and joints of the fingers and thereby facilitate strong and complete flexion of the digits in response to muscular contraction distant from the sites of mechanical action. Their anatomic arrangement in the second through fifth fingers is shown in Fig 1.
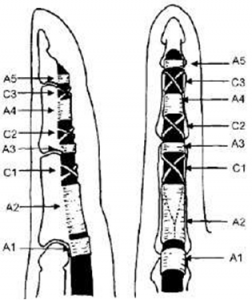
(Hauger 2000)
Fig 1. 2nd-5th finger pulley anatomy
Pulley anatomy of the thumb is somewhat different (Fig 2).
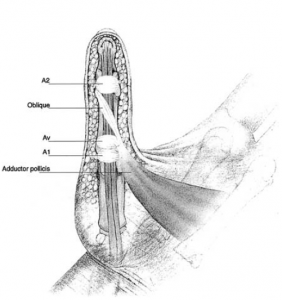
(Bayat 2002)
Fig 2. Thumb pulley anatomy
Some common anatomic variations of have been described as well (Bayat 2002).
Annular pulleys are classically subject to 4 main pathologies (Moutet 2003, Makkouk 2007):
- Trigger finger – chondroid metaplasia, usually of the A1 pulley, associated with stenosing tenosynovitis. Usually idiopathic, occurring in women in the 5th and 6th decades of life (F:M 6:1), most commonly thought to be due to a genetic predisposition. May also occur in rheumatoid arthritis, gout, diabetes mellitus (associated with duration of disease, not glycemic control), renal disease, amyloidosis, hypothyroidism, and connective tissue disorders. Ring finger most commonly affected, followed by thumb, long, index, and small fingers. Can be multiple.
- Tenosynovial ganglions – arise more commonly at a weak point between the A1 and A2 pulleys.
- Traumatic/surgical injuries to the tendon sheath.
- Overuse or stress ruptures of the annular pulleys, e.g. classically with rock climbing, but more recently shown in baseball pitchers too (Lourie 2010). Rock climbers typically injure distal aspect of the A2 pulley, with involvement of A3 and A4 in more severe injuries, related to crimping posture (DIP hyperextension and PIP hyperflexion). Baseball pitchers were shown in a small series to suffer isolated middle finger A4 injuries, thought to be related to repetitive ball-induced extension moments on an acutely flexed DIP joint when throwing fastballs (Lourie 2011). A2 pulley injuries have also been described in bowlers (Patel 2012).
#1 and #4 will be covered in this article.
Normal Anatomy
Annular and pulleys are arranged as in Fig 1, and are thin markedly hypointense structures on MR imaging connecting the flexor tendons to the phalanges and joints, best directly visualized on axial images. Cruciform pulleys are only rarely visualized on imaging due to their extremely small size.
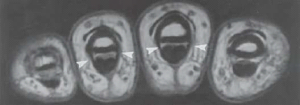
Fig 3. Arrowheads depict annular pulleys in cross section
On sagittal images, the next most useful images to evaluate for pulley injuries, the flexor tendons should be 1mm or less away from their adjacent phalanges.
Finger Pulley Injuries
With the rise in popularity of the sport of rock climbing in the 1980’s, closed finger pulley ruptures began to appear. Competitive climbers routinely put their entire body weight (and more during maneuvers) on one or two flexed fingers. Pulley lesions have been shown to be the single most common injury in these athletes (Schoff 2003).
Pulley lesions are most commonly seen in the ring and middle fingers and may be diagnosed in up to 30% of finger injuries. Fixed contracture of the PIP joint may result if timely diagnosis and treatment is not rendered.
Imaging is performed to clarify the severity and extent of pulley injury, as well as to exclude mimics such as tenosynovitis, tendon tear, or adjacent osseous or soft tissue injury. In young sport climbers, imaging is advisable to exclude epiphyseal fracture and epiphysiolysis (Hochnolzer 2005), preferably with both radiographs and MR as complementary modalities. CT should be reserved for problem-solving in cases of questionable fractures.
On sagittal MR and US images, more than 1mm of separation between the flexor tendons and phalanges is abnormal and is termed “bowstringing”, the extent of which generally reflects the severity and extent of the injuries, e.g. 2-5 mm in isolated complete single pulley ruptures, and 5-8 mm in simultaneous complete tears of multiple pulleys. Partial tears of annular pulleys result in bowstringing as well, typically to a lesser extent. Forced flexion is an important maneuver to elicit increase bowstringing in subtle cases. This may be much easier to image on focused ultrasound examination compared to MRI, due to the ease of provocation and much shorter required duration of flexion (which is often painful for injured patients).
Pulleys are seen to be either frankly torn in the case of a rupture, or thickened, thinned, and/or indistinct in the case of partial tears. Bowstringing is appreciable on sagittal as well as axial images.
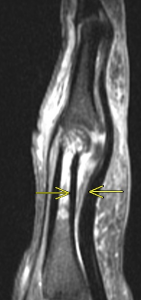
Fig 4a. Complete rupture of the A2 pulley (a – sagittal T2 fat-saturated MRI, b – axial T2 fat-saturated MRI ). Arrows depict bowstringing related to complete rupture of the A2 pulley
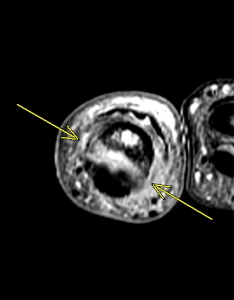
Fig 4b. Complete rupture of the A2 pulley (a – sagittal T2 fat-saturated MRI, b – axial T2 fat-saturated MRI ). Arrows depict bowstringing related to complete rupture of the A2 pulley

Fig 5a. Partial tear of A2 pulley. Arrows depict mild bowstringing related to partial tear of A2 (Clavero 2002) (a – sagittal MRI, b – axial MRI).
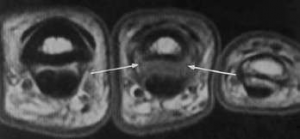
Fig 5b. Partial tear of A2 pulley. Arrows depict mild bowstringing related to partial tear of A2 (Clavero 2002) (a – sagittal MRI, b – axial MRI). Arrows depict attenuation and indistinctness of the medial and lateral aspects of the A2 pulley in T1 weighted images, consistent with partial tear.
Schoff (2006) classified pulley inuries in rock climbers as follows:
Grade I – Pulley strain
Grade II – Complete rupture of A4 or partial rupture of A2 or A3
Grade III – Complete rupture of A2 or A3
Grade IV – Multiple ruptures as A2/A3, A2/A3/A4, or single rupture (A2 or A3) combined with lumbricalis muscles or collateral ligament trauma. Current concepts favor surgery only in the case of a Type IV injury.
Trigger Finger
The A1 pulley is subjected to the highest stresses of all the pulleys, during normal and power-grip due to its location. Repeated threading of the flexor tendons through the A1 pulley can cause friction and result in intratendinous swelling, similar to fraying of a string with repeated threading through the eye of a needle. Electron microscopy has revealed fibrocartilagenous metaplasia and Type III collagen proliferation coating the pulley’s innermost layer as the precipitating pathologic lesion (Makkouk 2007).
Usually diagnosed clinically, trigger finger is imaged to localize the anatomic lesion and evaluate for rare mimics and associated pathologies, such as partial tendon tears or adhesions, or nodular tendinosis. MRI and US both demonstrate findings of thickening and inflammation of the A1 pulley, and post-gadolinium contrast images may demonstrate pulley enhancement, as in Fig 6..
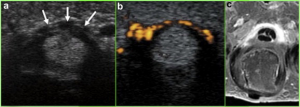
Fig. 6. Arrows depict A1 pulley hypertrophy on US, with Power Doppler demonstrating hyperemia, and post-contrast T1 fat-suppressed MRI demonstrating pulley enhancement (Vuillemin 2012)
Nodular tendinosis may be associated (Fig 7).
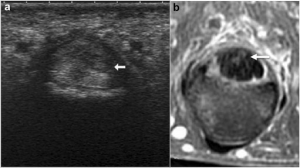
Fig 7. Arrows depict hypoechoic nodule on US, hyperintense on T2-weighted MRI (Vuillemin 2012)
Tenosynovial fluid and membrane thickening may also be seen, as with other stenosing tenosynovial processes such as De Quervain’s syndrome.
Traditionally treated with splinting, clinically guided corticosteroid injection, or surgical release, success with ultrasound-guided corticosteroid injection has also recently been reported, with 90% success rate in at 12 months, and 71% at year 3 (Bodor 2009).
Conclusion
Patterns of traumatic and non-traumatic pathologies of the finger pulleys are diverse, and important to recognize and accurately classify on imaging. Understanding these patterns is crucial to accurate and timely diagnosis to avoid complications, and to minimize time away from competitive or recreational activities.
All-American Teleradiology provides rapid, accurate decisive musculoskeletal MRI interpretations performed by highly experienced, fellowship trained Musculoskeletal Radiologists. Our value added consultative MRI services, to include our providing free MRI accreditation assistance and a Medical Director can help ensure appropriate reimbursement and the highest level of clinical performance.
For more information, email info@allamericanrad.com, call 888-365-5514 or visit www.allamericanrad.com.
Peter Louis Glickman, M.D.
Musculoskeletal Specialist, Foot & Ankle
All-American Teleradiology
Mark E. Pruzansky, M.D.
Assistant Clinical Professor of Orthopaedic Surgery
Icahn School of Medicine at Mount Sinai, New York, N.Y.
References
- Bayat A, Shaaban H, Giakas G, Lees VC. J Hand Surg Am. 2002 Jul;27(4):628-35. The pulley system of the thumb: anatomic and biomechanical study.
- Bodor M, Flossman T. J Ultrasound Med. 2009 Jun;28(6):737-43. Ultrasound-guided first annular pulley injection for trigger finger.
- Clavero JA, Alomar X, Monill JM, Esplugas M, Golanó P, Mendoza M, and Salvador A. Radiographics March 2002 22:2 237-256. EDUCATION EXHIBIT – Continuing Medical Education: MR Imaging of Ligament and Tendon Injuries of the Fingers.
- El-Sheikh Y, Wong I, Farrokhyar F, and Thoma A. Can J Plast Surg. 2006 Winter; 14(4): 227–231. PMCID: PMC2686056 Diagnosis of finger flexor pulley injury in rock climbers: A systematic review.
- Hauger O, Chung CB, Lektrakul N, Botte MJ, Trudell D, Boutin RD, Resnick D. Radiology. 2000 Oct;217(1):201-12. Pulley system in the fingers: normal anatomy and simulated lesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath.
- Hochholzer T, Schöffl VR. Wilderness Environ Med. 2005 Fall;16(3):139-42. Epiphyseal fractures of the finger middle joints in young sport climbers.
- Klauser A, Frauscher F, Bodner G, Halpern EJ, Schocke MF, Springer P, Gabl M, Judmaier W, zur Nedden D. Radiology. 2002 Mar;222(3):755-61. Finger pulley injuries in extreme rock climbers: depiction with dynamic US.
- Lourie GM, Hamby Z, Raasch WG, Chandler JB, Porter JL. Am J Sports Med. 2011 Feb;39(2):421-4. doi: 10.1177/0363546510387506. Epub 2010 Dec 20. Annular flexor pulley injuries in professional baseball pitchers: a case series.
- Makkouk AH, Oetgen ME, Swigart CR, and Dodds SD. Curr Rev Musculoskelet Med. 2008 June; 1(2): 92–96. Published online 2007 November 27. doi: 10.1007/s12178-007-9012-1 PMCID: PMC2684207 Trigger finger: etiology, evaluation, and treatment.
- Moutet F. Chir Main. 2003 Feb;22(1):1-12. [Flexor tendon pulley system: anatomy, pathology, treatment]. [Article in French]
- Patel P, Schucany WG, Toye L, and Ortinau E. Proc (Bayl Univ Med Cent). 2012 July; 25(3): 282–284. Flexor tendon pulley injury in a bowler.
- Schöffl VR, Schöffl I. J Hand Surg Am. 2006 Apr;31(4):647-54. Injuries to the finger flexor pulley system in rock climbers: current concepts.
- Vuillemin V, Guerini H, Bard H, Morvan G. J Ultrasound. 2012 Feb;15(1):20-8. doi: 10.1016/j.jus.2012.02.002. Epub 2012 Mar 9. Stenosing tenosynovitis.

